The General Medical Council has (GMC) published ‘The state of medical education and practice in the UK: the workforce report 2022.’ This highlights statistical trends and challenges facing the medical workforce, including specific data on the ophthalmology workforce. RCOphth Policy Manager Jordan Marshall and Policy Advisor David Murray summarise the key findings and what they mean for ophthalmology.
As the regulator for doctors across the UK, the General Medical Council (GMC) is well placed to analyse workforce trends based on who is joining and leaving its registers. They are explicit in this report on the medical workforce that they intend for their analysis to ‘inform workforce planning across the UK’.
Commenting on the report, RCOphth President Professor Bernie Chang said:
“This report highlights important key trends behind the lack of workforce capacity in ophthalmology. Slow growth in the number of ophthalmologists is a key reason why tackling backlogs and meeting patient demand in a timely way is so challenging in many parts of the UK. It is essential that we see increases in the number of ophthalmology training places to provide this capacity for the long term. Growing numbers of SAS doctors have however provided an important boost for ophthalmology services. Supporting their progression, as well as efforts to upskill other professions in the multi-disciplinary eye care workforce will also be crucial in increasing our capacity to deliver patient care”.
Key points from The state of medical education and practice in the UK: the workforce report are:
- The medical workforce grew by 17% between 2017-2021, largely due to a 40% increase in SAS and LE doctors. SAS doctors are a vital part of the ophthalmic workforce, and it is important they are given opportunities to develop their careers within ophthalmology.
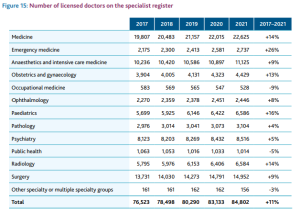
- The number of ophthalmologists increased by 8%, compared to a slightly higher average of 11% across all specialties on the specialist register.
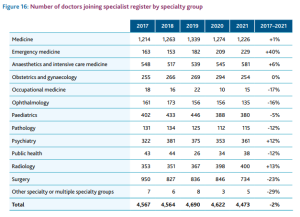
- The report highlights potentially worrying trends in both the number of ophthalmologists joining the register and those leaving. There was a 13% fall in those joining the ophthalmology register between 2020 and 2021. This may be partly attributable to the impact of training being disrupted during the pandemic, as we highlighted in our analysis earlier this year of GMC’s National Training Survey.
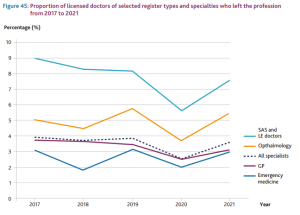
- Over the last five years, there has been a 20% increase in those leaving the ophthalmology specialist register – compared to a 3% increase across all specialties. Some of this pattern may be due to the age profile of the ophthalmology workforce – almost half of ophthalmologists (47%) were over the age of 50 in 2021. The report worryingly also found that of those ophthalmologists who gained their Certificate of Completion of Training (CCT) in 2013, 13% had left the register by 2021.
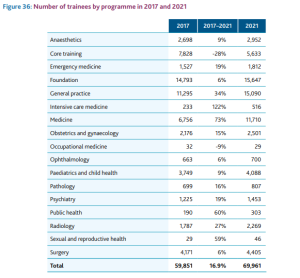
- A lack of increase in training posts in ophthalmology over the last decade has been an important factor in contributing to the slow growth in ophthalmologists joining the register. GMC highlights that there has been a 6% growth in ophthalmology training posts over the last five years, compared to 17% across all specialties. That picture should begin to shift in the coming years following the welcome announcement that there will be 15 extra ophthalmology training posts in 2022/23. This commitment now needs to be delivered and we will continue to make the case for further increases in the coming years to meet patient need, as well as for support for routes that enable the existing multi-disciplinary ophthalmic workforce to upskill such as Ophthalmic Practitioner Training.
- There has been a very large increase in International Medical Graduates (those from outside the European Economic Area) practising in the UK – a 121% rise in IMGs joining the workforce since 2017. IMGs who joined the workforce outnumbered UK and European Economic Area (EEA) graduates in 2021.
Ophthalmology workforce capacity risks falling behind patient need on current trends
The medical workforce is growing, with the majority of specialties – including ophthalmology – on the medical register increasing in size since 2017. While the overall increase of 8% in the number of ophthalmologists is welcome, this is low compared to other specialties and does not represent the pace of growth needed to match either the estimated increase in demand of 40% over the next 20 years or to tackle current ophthalmology waiting lists across the UK.
Key trends include:
- The increase in the number of licensed ophthalmologists on the specialist register was below the average across specialties, increasing by 8% compared to an average of 11% (see Figure 15 below from the GMC report). Some specialties have seen particularly large increases (emergency medicine and paediatrics), while two have actually seen falls (occupational medicine and public health).
- There was a 16% decrease in the number of ophthalmologists joining the specialty compared to an average drop of 2% across all specialty groups (see figure 16 below from the GMC report). This drop was almost entirely between 2020 and 2021, suggesting the impact of the pandemic in delaying progression from training. This is an issue we highlighted in our analysis earlier this year of GMC’s National Training Survey.
- More doctors leave ophthalmology compared to other specialties. Figure 45 below from the GMC report shows that in most years between 2017-2021, 5-6% of ophthalmologists left the register. This is higher than the average across all specialties, which generally tracked at between 3-4%. Part of this trend will be due to retirement and the consultant ophthalmology workforce having a higher age profile than other specialties. Almost half (47%) of ophthalmologists were over the age of 50 in 2021. But GMC also found that of those ophthalmologists who gained their CCT in 2013, 13% were no longer on the register at the end of 2021. This figure is concerning, although it is lower than a number of other specialties with obstetrics and gynaecology, psychiatry and radiology among those with higher leaving rates. Figure 45 also shows that SAS and LE doctors leave the workforce in higher numbers than all other groups – GMC says this is largely due to ‘many having joined on fixed term arrangements but…there could be an opportunity to retain more of these doctors for longer’.
- Ophthalmology saw a relatively slow expansion in the number of trainees between 2017 and 2021 – see Figure 36 below from the GMC report. Ophthalmology trainees increased by 6% over those four years, compared to an average of 17% across all other specialties. This picture should begin to shift in the coming years following the welcome announcement that there will be an extra 15 ophthalmology training posts in 2022/23. We will continue to make the case for further increases in the coming years.
Overall workforce trends highlight the rising profile of SAS and IMG doctors
While the number of doctors joining the workforce overall has grown by 17% over the last five years, that growth is not consistent, varying considerably between type of doctor, specialty, ethnicity of the doctor and UK nation. Key trends include:
- The number of SAS and LE doctors on the GMC register has increased by 40% since 2017. If the trend continues, by 2030 SAS and LE doctors in secondary care will form the largest group in the medical workforce. Linked to this trend is the rise in international medical graduates (IMGs) from outside the UK and other European nations – also up by 40% since 2017.
- England and Wales have had 16% and 15% increases in their medical workforce since 2017, while the figures for Northern Ireland and Scotland are 10% and 9%. GMC links this divergence to the higher proportion of IMGs in England and Wales.
- The gender balance of the workforce continues its long term-trend towards parity. In 2021, more females than males joined the GMC’s registers. 51% of the medical workforce was male in 2021, compared to 53% in 2017. This trend will continue given 64% of the medical student intake was female in 2021/22, and greater proportions of those nearing retirement age are male. 66% of ophtahlmologists are male, down from 74% in 2012. All specialties, including ophthalmology, had an increasing female composition between 2012-2021. Of those in the ophthalmology training programme, just over half (53%) are now male, compared to 57% in 2012.
- There has been a very large increase in International Medical Graduates (IMG) practising in the UK. UK graduates joining the workforce rose by 2% from 2017, compared to a 121% rise in IMGs. IMGs who joined the workforce outnumbered UK and European Economic Area (EEA) graduates in 2021, with doctors from South Asia, the Middle East and Africa driving this increase.
- There has been a 67% increase in doctors who are Black or Black British on the GMC’s registers since 2017 – although this is from a low base – still only 6% of those who specify their ethnicity are Black or Black British. There was also a 30% increase in those from Asian or Asian British backgrounds. Asian or Asian British doctors now comprise 31% of the medical workforce. 57% of the ophthalmologist workforce who specify their ethnicity are White, with 34% Asian or Asian British and 2.3% Black or Black British. Since 2012, those who are Asian or Asian British and Black or Black British have increased by over 50%. However for the latter, this was from a very low base – there are still only 53 ophthalmologists in the UK who identify as Black or Black British. Of ophthalmologists in training, 46% are Asian or Asian British, 38% are White and 2.9% are Black or Black British. These trends have changed little since 2012.
- The average age of retirement has remained at just under 64 over the last ten years, with no evidence of doctors retiring earlier. The most common reason for leaving the register cited by those with a UK Primary Medical Qualification (PMQ) was retirement. For non-UK PMQ doctors, the most cited factor was leaving to practise abroad. Most non-UK PMQ doctors who wanted to practise abroad returned to their respective countries of nationality while British doctors practicing abroad stated their plans were to move to an English-speaking country, such as Australia, New Zealand or Canada.
Conclusion and next steps for the College
One of the key trends the GMC highlighted in this report was the growing role played by SAS doctors. As well as describing these trends, GMC outlines how through legislation they want to support SAS doctors to work in general practice and progress in specialties. They go on to say that ‘we are actively involved in conversations about how training pathways can be made more accessible and how progression routes could evolve beyond the traditional path to consultant or general practice. Legislative change is coming that will provide us with more flexibility and autonomy in designing less intensive ways of recognising SAS doctors’ skills, enabling them to join the GP or specialist registers’.
These plans are at a very early stage. We have had an initial conversation with the GMC and will share more detail and consult within the College when these plans are more developed. RCOphth is committed to ensuring that SAS doctors are offered opportunities to progress and develop their careers. The new ‘specialist’ grade contract agreed last year will also help to support such progression.
The other key issue that this GMC report illustrates is that the capacity of the ophthalmology medical workforce has increased sluggishly over recent years, especially compared to many other specialties. This is a key reason why it is now difficult to tackle the backlogs that have arisen after COVID-19. Almost 650,000 people are on the waiting list for ophthalmology treatment in England. This is nearly 10% of the entire NHS backlog in England, and has increased by 44% compared to before the pandemic. In Scotland, the number of patients waiting for an ophthalmology outpatient appointment has almost doubled since 2019 and in Northern Ireland over half of patients are waiting over a year for an outpatient appointment.
As RCOphth continues to emphasise to policymakers (for example in our response to a Health Education England call for evidence in 2021), we need to increase the number of ophthalmology training places to ensure the long term capacity to meet patient need is there. The plans to increase the number of training places by 15 in England in 2022/23 need to be delivered, and further increases will be needed in future years, in line with the increase in medical school places, to allow ophthalmology to keep up with patient demand. We also need more backing for routes that enable the existing multi-disciplinary ophthalmic workforce to upskill such as Ophthalmic Practitioner Training. NHS organisations also need to support the creation of more ophthalmic technician and imaging grader roles that can help to increase capacity quickly, especially in the context of a shift towards virtual outpatients and community diagnostic hubs.
If you have any questions or comments on our analysis, please contact [email protected]. The GMC’s full report The state of medical education and practice in the UK: The workforce report 2022 can also be explored further.